Posted January 18th 2021
The COVID–19 pandemic has been challenging for everyone and we all respond differently to living through such a strange and stressful time.
Common, normal reactions have included at times positive feelings of hope and togetherness alongside negative emotions of worry and anxiety.
Professor Jonathan Bisson, whose main research interests are in the field of post-traumatic stress, introduced the work of NCMH’s latest research findings as part of Cardiff University’s Science in Health online webinar series in December 2020.
Understanding the results
The COVID-19 study launched in the summer of 2020 and over 3,000 responses were received from the Centre’s cohort of adult participants with a history of mental illness.
The data, whose analysis was led by Dr Katie Lewis, focused questions on an individual’s experiences relating to the pandemic, how they felt it had impacted on their mental health and aimed to measure their overall well-being as a result.
The participants had a variety of mental health diagnoses including anxiety disorders, depressive disorders, Post-traumatic Stress Disorder (PTSD) and eating disorders.
The varied disorders also enabled analysis of these specific mental health experiences in relation to the general population.
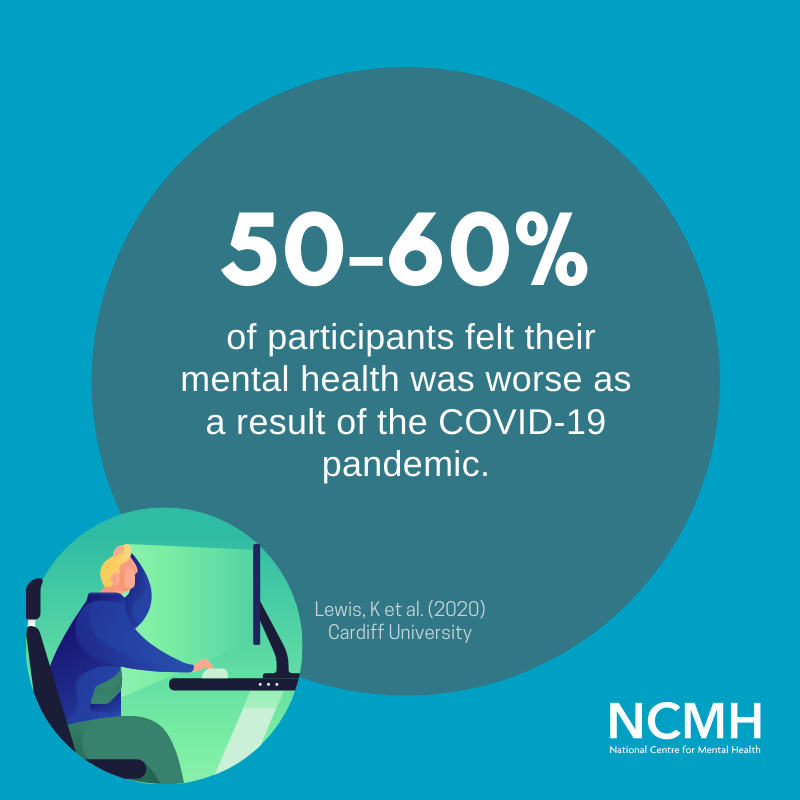
The data revealed that high levels of people described their well-being as poor with 50-60% answering that they felt worse as a result of the pandemic.
Interestingly, however, 10% of participants said they felt much better during the pandemic.
Individuals said that the restrictions brought in through national lockdowns enabled them to not be regularly exposed to the outside world which they ordinarily find anxiety-provoking.
Others said the restrictions helped them feel more at ease and similar to others as everyone else was in the same position in not being able to go out either.
The summer survey also provided an opportunity to examine the impact of contextual factors on participants such as age, low income, sleep patterns and increased alcohol and substance use.
The survey resoundingly highlighted the increased difficulty caused by the pandemic in accessing mental health services and not being supported as easily by friends and family networks.

Professor Bisson, above, said “Lack of mental health professional support over lockdown has been one of the most difficult factors we found in our cohort.
“We have evidence at this stage that the lack of accessible mental health services has had an impact.
Not being able to see people, both within a personal and professional support network, in the usual way, as well as long waiting lists for psychological treatments has added to the struggles for many.
“That’s why NCMH are looking at alternative techniques like guided self-help which would enable treatments to be given in a timely manner to reach more people.”
COVID-19 and PTSD
The finding of NCMH’s most recent survey was completed at the end of 2020.
The Post–Traumatic Stress Disorder survey asked the same people that were surveyed earlier in the year but this time with questions looking specifically at PTSD diagnoses in relation to the pandemic.
Around 40% of individuals surveyed found at least one aspect of the Covid-19 crisis to be traumatic.
The most common concern given by participants with lived experience of mental health difficulties was general worry about the pandemic followed by lockdown restrictions. Other people not following the rules appeared a source of unease, as well as using face coverings, news and media coverage, governments handling of the pandemic, financial concerns and fear of catching the virus itself.

The data poses further questions on how the COVID–19 pandemic may fit in the classification of PTSD traumatic events.
Prof Bisson added, “Most of these listed concerns are interestingly not things we would be looking at as traumas in terms of post-traumatic stress disorder.
“Based on psychiatric definitions of trauma, living through the pandemic would not be enough to fulfil the criteria and thus be categorised as a PTSD traumatic event.
This is an interesting discussion point for debate, and we are looking forward to exploring this further.”
The survey results showed that only 1% of participants fit the strict criteria for identifying trauma and were probable of suffering PTSD as a result of COVID-19.
With this in mind, Prof Bisson went on to say that: “We are still in the midst of a global pandemic and following up to discover the longer-term mental impacts will be crucial.
This pandemic is different to a one-off trauma event and is much more akin to flooding, for example.
“The impact of flooding has a longer-term, depressive flavour rather than a PTSD flavour. I am expecting we will see a similar outcome over time because of this crisis. This will allow us to learn more about the lasting effects of ‘long Covid’ from people who have had the virus themselves.”
So where next for this study?
NCMH intend on following up longitudinally through further analyses of this preliminary data to gather a better understanding of the longer-term mental health impact of the pandemic.
Researchers are currently developing follow-up COVID-19 surveys on sleep, eating disorders and OCD.
The Centre is also looking to develop guided self-help interventions for conditions likely to be exacerbated by COVID-19, such as Prolonged Grief Disorder (PGD) and complex PTSD.
To view Professor Bisson’s full lecture, please visit the School of Medicine’s Youtube
Take part in our research
- General online study
- COVID-19 study for people living with mental health problems
- COVID-19 and people with learning disabilities study
- Premenstrual Dysphoric Disorder
Read more
- Bereavement during the COVID-19 pandemic – developing a new treatment for Prolonger Grief Disorder
- Neuroswipe – swipe right to help with brain research from home
- Children’s mental health during the COVID-19 pandemic
- NCMH mental health leaflets
Sign up now and receive new blog posts to your inbox.
